The Fundamentals of Insulin Injection Therapy
Insulin, a hormone secreted by the pancreas, works primarily by reducing blood sugar levels. When bound to insulin, it triggers the release of glucose transporters in the cell membrane. Glucose can enter cells freely from the bloodstream after being unblocked by insulin at glucose transporters.
If you have insulin dependence, you must take insulin injections every day or risk serious health complications. If you have type 1 diabetes, your pancreas isn’t producing any insulin, and if you have type 2 diabetes, the insulin your pancreas does produce isn’t working properly.
A Primer on Insulin
Before we go into the different insulin schedules, I need to define two concepts you will hear often:
Injectable long-acting insulin that simulates pancreatic insulin secretion is known as basal insulin. The insulin in a single basal dose continues to work slowly throughout the day, reducing insulin injection frequency to once or twice daily. Unlike fast-acting insulins, which cause a sharp drop in blood sugar, these long-acting insulins are “peakless,” meaning they aim to keep glucose levels constant throughout the day.
Insulin bolus – in medicine, a “bolus” refers to a single injection. The quick rise in blood glucose after eating necessitates the administration of bolus insulin. Some bolus insulins might begin lowering blood sugar levels within minutes of being administered. They don’t hang around for long, as the body breaks them down and flushes them out in a matter of hours.
In conclusion, basal insulin maintains steady blood sugar levels in the absence of food, but a bolus of fast-acting insulin is required to counteract the rapid spike in blood sugar caused by the digestion of carbohydrates.
When Should Insulin Be Given?
Patients with type 1 diabetes always require insulin therapy due to an absolute lack of the hormone. Until the condition has progressed to the point where the patient is very resistant to insulin or when oral antidiabetic drugs are no longer sufficient to keep blood glucose levels down, insulin is usually not necessary for type 2 diabetics.
Patients with insulin-dependent type 2 diabetes are required to inject insulin much like those with type 1. Type 2 diabetics, on the other hand, have developed insulin resistance and typically require significantly higher insulin doses than type 1 diabetics.
To help the body’s own insulin do its work, many people with type 2 diabetes find that taking an additional long-acting (basal) insulin like Lantus or Levemir is sufficient. If it isn’t enough, you can also take fast-acting insulin boluses before meals together with a basal dose.
Insulin Concoctions
One common pre-mixed variety is called humulin or mixture and contains 70% long-acting and 30% fast-acting ingredients. These are commonly consumed in the hours prior to breakfast and dinner.
Although administering premixed insulin is convenient, the combination of basal and bolus injections provides far better glucose control and is a more adaptable strategy. This is because the bolus may be adjusted in size and timing to accommodate a wide range of mealtimes and food types.
Combinations of insulin, such as the 70/30 mix, require strict adherence to dosing schedules and carbohydrate intake limits. Due to the combination of slow and fast-acting insulin, you cannot adjust the timing of your injections, and you also cannot adjust your caloric intake based on how hungry you are.
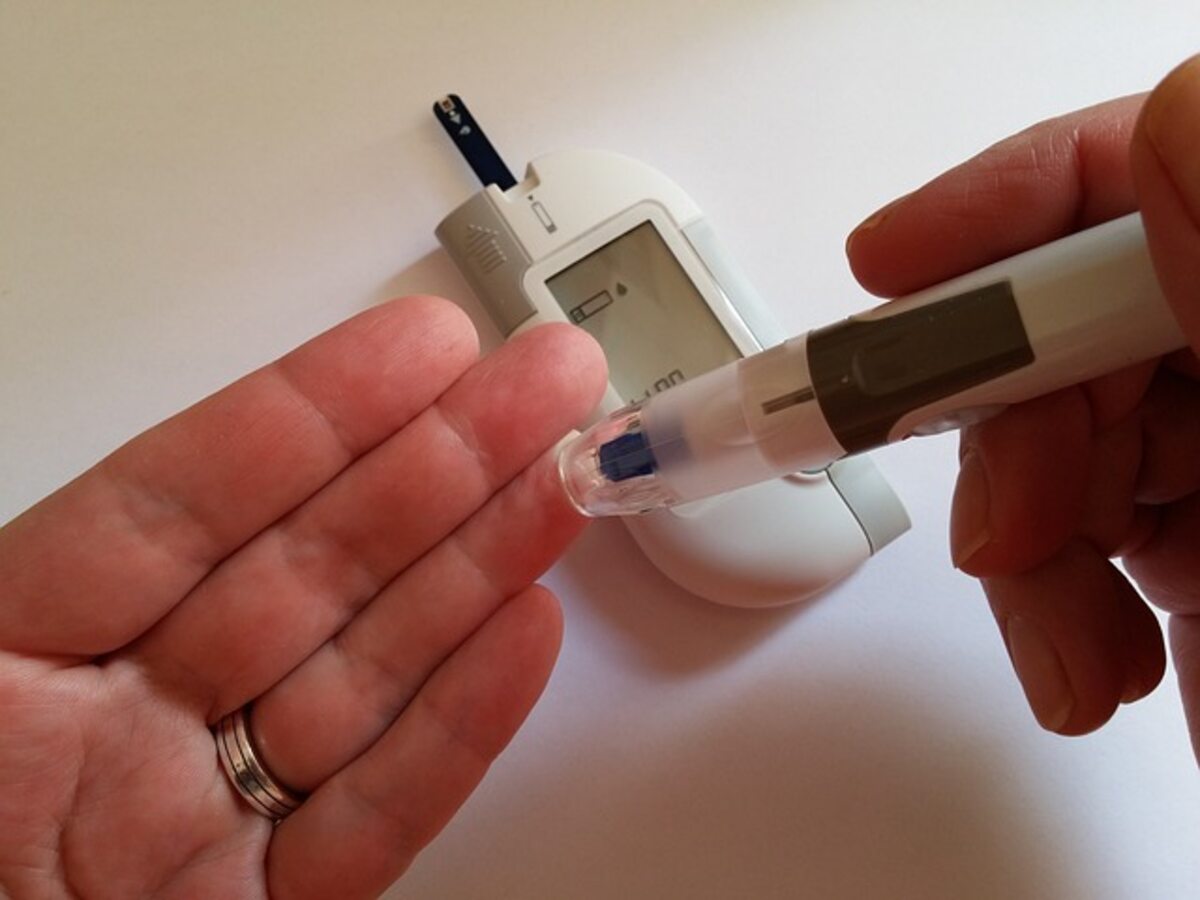
Insulin Injection Procedure
Injecting insulin with a conventional syringe may be necessary if your doctor has prescribed a very stringent insulin regimen. However, these days most patients utilize injection pens that come pre-filled with insulin because they are considerably more convenient. The following fundamentals hold true in either scenario:
To prevent any particles from sinking to the bottom of the syringe, step one involves rolling the insulin vial (or the syringe itself, if it has been pre-filled) several times between the palms of your hands. This guarantees that each dose contains the same amount of insulin. Insulin pens should be shaken similarly, as most of them have a little glass ball that can move around and mix the insulin thoroughly if shaken.
Second, pinch the skin at the desired injection spot. Put the needle of the syringe or pen under the skin’s fatty layer to inject the insulin. Keep in mind that a 45-degree angle is ideal for very skinny kids and adults, while a 90-degree tilt is better for everyone else.
Third, swap out your injection sites on a regular basis. Rotating injection sites in the abdomen are good because insulin is best absorbed there. Imagine a grid of 8 squares covering your stomach. Give each square a day of the week, then switch them around every day.
Tips for Injecting Insulin
First, at least an inch should be left between each subsequent injection.
Injecting into clean skin eliminates the need for an alcohol swab to prevent infection at the injection site.
Insulin can be injected through clothing if necessary, though this is not recommended.
Never shake an insulin vial, as doing so can cause air bubbles that will prevent the syringe from being properly injected.
5. Insulin of different types should never be used in the same syringe. This can cause its effects to be unpredictable.
6. Avoid injecting insulin into skeletal muscle if at all possible. It hurts, and it causes hypoglycemia because the insulin is absorbed too quickly.
Infusion Systems
Type 1 diabetes [http://www.bloodsugarsimplified.com/type-1-diabetes/type-1-diabetes mellitus/] typically requires the use of an insulin pump. however, they can be just as helpful for people with type 2 diabetes who are insulin dependent.
Using an insulin pump has a number of benefits.
If you have a fear of needles, insulin pumping is preferable to daily injections because you only have to replace the infusion site every three days.
Using an insulin pump will allow you to reduce your daily insulin dose. Fast-acting insulin, which pumps utilize exclusively, is more effective than slower-acting insulins. Using an insulin pump can reduce your insulin consumption by up to 20%.
If you are motivated, you can achieve considerably lower HbA1c (glucose average) than with injections since you have more control over the amount of insulin you take. The ability to take fractional rather than whole units allows for greater dosing precision.
The artificial pancreas represents a significant advance in the field of insulin pumps. Automatically calculating your insulin requirements minute by minute, this device combines an insulin pump and a continuous blood glucose meter. Although the JDRF and other organizations have poured significant resources into research and development, this product is not yet available to the general public. Trials in humans are currently being conducted.
Is an Insulin Pump the Best Option for Me?
Pump therapy is often reserved for those with type 1 diabetes or insulin-dependent type 2 diabetes, therefore it is not an option for everyone. Using an insulin pump effectively requires:
You must be proficient at keeping track of your carb intake. Putting your planned carbohydrate intake into the pump is a laborious process. Next, it determines how much insulin you need.
You should feel at ease in a technological environment. You shouldn’t use an insulin pump if you can’t use a simple device like a cell phone. This is obviously not the case, though, as you are probably reading this on a computer.
You’ll need some patience to give the pump a fair go at winning you over. Normal blood glucose levels often take at least a week or two to be achieved. After that, you’ll need to practice adjusting the device for at least a few more weeks before you feel comfortable doing so.
You need to maintain composure rather than panic. When your blood sugar starts to creep up, you need to act fast to figure out what’s wrong and how to fix it. The delay between noticing a problem and seeking aid is too long for another person to manage your pump for you, so while your doctor can help you get started, you’ll ultimately have to figure out how to use the device on your own.
Last but not least, you’ll need to be willing to use a glucometer to check your blood sugar levels multiple times daily and more frequently than that while making changes to your routine.
Irish endocrinologist Dr. Michael Murphy. He has worked with diabetic patients for many years and has a wealth of information on the subject.
For advice from a real-world endocrinologist, check out BloodSugarSimplified.com. All your questions regarding diabetes are answered in clear, up-to-date articles.
Read also: Unlocking New Frontiers In Health And Wellness With In-Home Care